Case 21 - Veggies Gone Off
Author: Nish Cherian Reviewer: Gokul Sagar
A female in her 30’s is brought to the ED with a reduced level of consciousness. She looks unwell and has signs of a head injury. She is tachycardic with a small O2 requirement. A trauma pan-CT is performed showing no obvious traumatic injuries but infarcts in the spleen, kidney and brain, suspicious for a septic or embolic source. The patient deteriorates with an increasing O2 requirement and decreasing GCS and is admitted to the ICU. A focused echo is performed:

Clips 1-4: Parasternal long axis (PLAX) 2D, aortic valve focused, Colour Doppler over MV and AV.
Clips 5-8: Parasternal short axis (PSAX) of LV and AV and apical 4-chamber.
During the echo, the patient deteriorates further and is rapidly intubated for worsening respiratory failure. Post-intubation she is hypotensive with escalating noradrenaline requirements. Enoximone is added in for additional inotropy. A more detailed assessment of stroke volume, RV pressures and AR severity is performed:
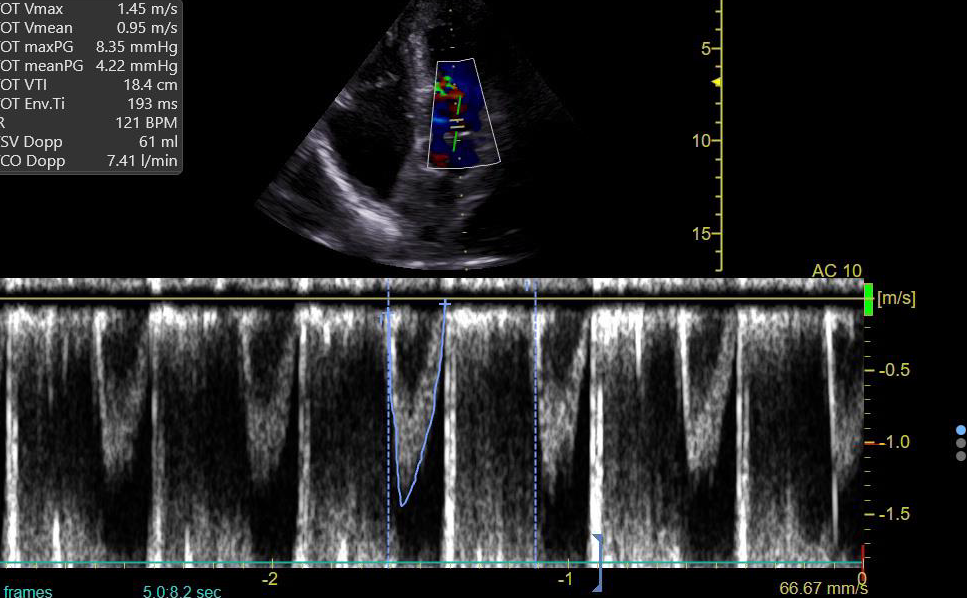

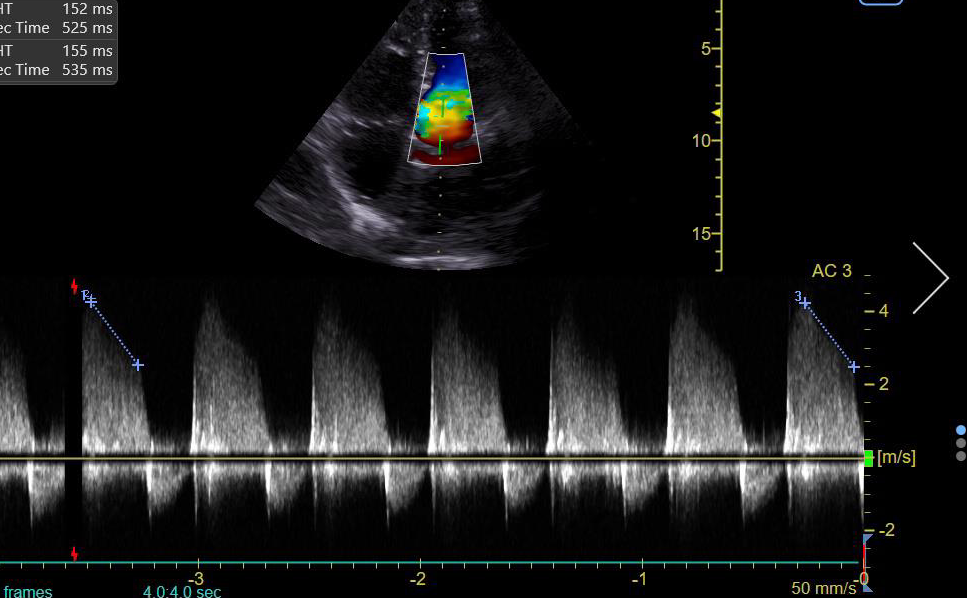
Clips 9-14: Apical 4-chamber (A4C) 2D and colour over MV and TV, LVOT VTI, TR velocity, LVOT pressure half-time (PHT).
-
Dilated LV cavity with impaired function (and hypokinetic inferolateral wall)
Mitral regurgitation
Thickened aortic valve highly suspicious vegetation, which appears to prolapse during diastole with significant regurgitation on colour flow.
Left basal consolidation
-
Non-coronary cusp
-
Vegetations - hallmark feature, typically an oscillating mass on valve (or other endocardial structure/implanted device).
Peri-valvular abscess - usually occurs in aortic valve IE and involve the mitral-aortic intervalvular fibrosa. Typically looks like a perivalvular zone of reduced echogenicity without colour flow. Other perivalvular complications include pseudooaneurysm and fistulae.
New dehiscence of prosthetic valve - identified by new paravalvular regurgitation (with or without rocking motion of prosthesis)
-
RVSP = 4V^2 + RAP
TR Peak velocity = 3.4 m/s (from Clip 12)
RAP = estimated at 15mmHg (based on IVC diameter >2.1cm with <50% collapse
So RVSP = 4 x (3.4^2) + 15 = 61 mmHg (which is high)
This would indicate an intermediate-high probability of pulmonary hypertension
-
PHT represents the time taken for the initial maximal pressure gradient across the AV to fall by 50% during diastole. The drop is steeper with increasing severity.
Mild AR = PHT >500ms
Moderate AR = PHT 200-500ms
Severe AR = PHT <200ms
This would be classed as severe AR (with PHT of 150ms).
-
Specific signs of severe AR
Central regurgitation jet of >65% of LVOT or vena contracta >0.6cm
Flail/wide coaptation defect of AV
Holodiastolic flow reversal in descending aorta
Diastolic MR (this tends to occur more in acute AR due to rapid rise in LV pressure during diastole causing pre-systolic closure of MV)
Supportive signs
Large flow convergence
Dilated LV with normal EF
Quantitative measures (eg. Reg volume/fraction, EROA) - should be interpreted in the context of other signs
-
LVOT VTI (velocity time integral) is a surrogate measure of SV and CO. The normal range is 18-22cm.
The LVOT VTI is measured here at 18.4cm which is technically in the normal range and would suggest normal SV/CO. However, in the context of moderate-severe AR, the LVOT VTI is usually higher than normal due to the increase in end-diastolic volume.
Therefore, LVOT VTI and SV/CO estimation can be inaccurate and misleading in such cases, as VTIs in the normal range may, in fact, represent a reduced cardiac output state for the patient.
-
Heart failure, perivalvular extension and embolic events are the most common severe complications of IE and also the main indications for early surgery.
European guidelines recommend surgery in acute regurgitation with heart failure and in patients with obstructive vegetations.
Embolic events carry a high risk of morbidity and mortality. Echo can evaluate the number and size of vegetations which can help to predict embolic risk and guide decisions for surgery to prevent embolism.
Follow up
The next day, there is no significant clinical improvement unfortunately. A comprehensive TTE is performed confirming the POCUS findings, though the LV is now more dilated and impaired with increasing LA filling pressures. The patient is discussed with the local Cardiothoracics centre but not felt to be a candidate for mechanical support/surgery due to extent of embolic infarcts in the brain (confirmed with MRI). A decision is made to withdraw life-sustaining therapy.
Final take home points
Despite its limitations, TTE is usually the first-line investigation performed in suspected IE as it is non-invasive. Sensitivity for vegetations is around 75% (compared to 85-90% with TOE) but specificity has been reported >90% for both TTE/TOE.
Bedside/focused TTE it is very useful, particularly in the critically unwell patient with a high pre-test probability of disease, and can help estimate severity, assess complications of IE and guide treatment decisions (eg. need for inotropic, mechanical support and surgery). It is important, however, that a comprehensive (“formal”) TTE/TOE is performed when feasible.
Be wary of interpreting LVOT VTI in the context of moderate-severe AR. It should normally be higher than normal, and values in the normal range can be misleading and not representative of the true SV/CO. Similarly, the LV function/EF is usually high initially with AR so you would expect to see a hyperdynamic LV (acutely).
Acute AR is life-threatening as the LV has not had time to develop compensatory mechanisms for the increased LV end-diastolic pressure and volume load - usually presents in a more haemodynamically compromised state with cardiogenic shock/pulmonary oedema. With time and more subacute/chronic AR, there is a compensatory increase in LV end-diastolic volume/cavity size in order to maintain an effective stroke volume.
Early involvement of Cardiothoracics is important to decide on whether early surgery is indicated.
ESC recommendations are a useful resource: https://www.escardio.org/static-file/Escardio/Subspecialty/EACVI/position-papers/recommendations-endocarditis.full.pdf
APPENDIX/RESOURCES
Aortic valve leaflets
Pitfalls of VTI: https://www.youtube.com/watch?v=TguP8GHHD88
ASE guidelines


